Hip Replacement Surgery
Indications for Hip Replacement
- Osteoarthritis: The most common reason, where the cartilage cushioning the bones wears down.
- Rheumatoid Arthritis: An autoimmune condition causing inflammation in the joints.
- Traumatic Arthritis: Resulting from an injury or fracture.
- Avascular Necrosis: A condition where bone tissue dies due to lack of blood supply.
- Hip Dysplasia: Abnormal hip joint development.
Types of Hip Replacement
- Total Hip Replacement (THR): Both the ball (femoral head) and the socket (acetabulum) are replaced.
- Partial Hip Replacement: Only the femoral head is replaced.
- Hip Resurfacing: The femoral head is capped with a smooth metal covering.
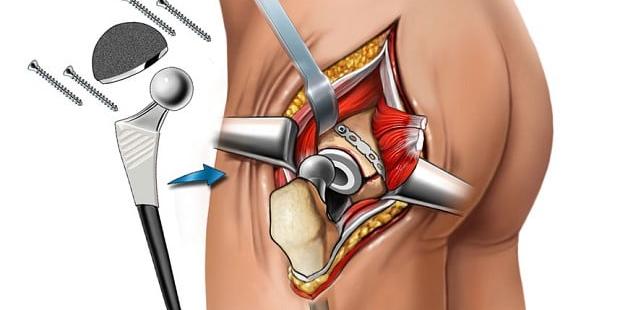
Components of a Hip Implant
- Acetabular Component: The socket part, which can be made of metal, ceramic, or plastic.
- Femoral Component: The stem that fits into the thigh bone, usually made of metal.
- Bearing Surface: The part that interfaces between the socket and the ball, made of various materials like metal, ceramic, or polyethylene.
The Procedure
- Preparation: Includes medical evaluation, imaging tests, and sometimes pre-surgical physical therapy.
- Anesthesia: General or spinal anesthesia is used.
- Incision: A cut is made over the hip to access the joint.
- Removal: Damaged bone and cartilage are removed.
- Implantation: The new artificial components are inserted.
- Closure: The incision is closed with stitches or staples.
Recovery and Rehabilitation
- Hospital Stay: Typically a few days, depending on the patient’s condition.
- Pain Management: Medication to control pain and prevent infection.
- Physical Therapy: Essential to restore movement and strength.
- Activity: Gradual increase in activities with certain restrictions to avoid dislocation.
- Follow-Up: Regular check-ups to monitor the implant.
Risks and Complications
- Infection: A risk with any surgery, managed with antibiotics.
- Blood Clots: Prevented with medications and physical activity.
- Dislocation: More common in the early post-operative period.
- Implant Wear and Tear: Over time, the artificial joint might need revision.
- Nerve Damage: Rare but possible.
Long-Term Outcomes
Most patients experience significant pain relief and improved function, with artificial hips typically lasting 15-20 years. Advances in materials and surgical techniques continue to improve outcomes and longevity of hip replacements.
Advances in Hip Replacement
- Minimally Invasive Surgery: Smaller incisions and faster recovery.
- Robotic-Assisted Surgery: Enhances precision in implant placement.
- Custom Implants: Tailored to individual anatomy using 3D printing.
Considerations Before Surgery
- Alternative Treatments: Physical therapy, medications, or less invasive procedures.
- Lifestyle Changes: Weight loss, exercise, and modifications in daily activities.
- Patient Education: Understanding the procedure, recovery, and realistic expectations.